Sports Physiotherapy SIG - SLKS

SLKS
Mission and Scope
The Luxembourg Society of Sports Physiotherapy (S.L.K.S.), a.s.b.l., founded in 1986, is affiliated with the Luxembourg Olympic and Sports Committee (C.O.S.L.) and a member of the International Federation of Sports Physical Therapy (IFSPT). It brings together physiotherapists who demonstrate advanced skills in the field of sports physiotherapy and currently has 93 members (2022). Its mission is to promote and develop the profession of sports physiotherapist, to inform and educate physiotherapists about advances in the fields of physiotherapy and sports medicine, and to protect clean sport by respecting the code of the World Anti-Doping Agency and its eight international standards. It aims to improve the quality of sports physiotherapy in Luxembourg in terms of knowledge, skills, and professional responsibility. The S.L.K.S. organizes and hosts scientific conferences, symposia, and technical workshops, and promotes the development of the profession by creating means of education and information. Furthermore, the S.L.K.S. represents its members to partner organizations and public authorities. Through its collaboration with sports clubs, federations, and the C.O.S.L., the S.L.K.S. encourages evidence-based practice and the highest quality of care for athletes of all ages and abilities by appointing physiotherapists trained and specialized in the field of sports physiotherapy.
Do not hesitate to consult the website https://sportkine.lu/

Les compétences requises pour un kinésithérapeute du sport sont reprises ci-dessous par l’I.F.S.P.T. (International Fédération of Sport Physical Therapist)
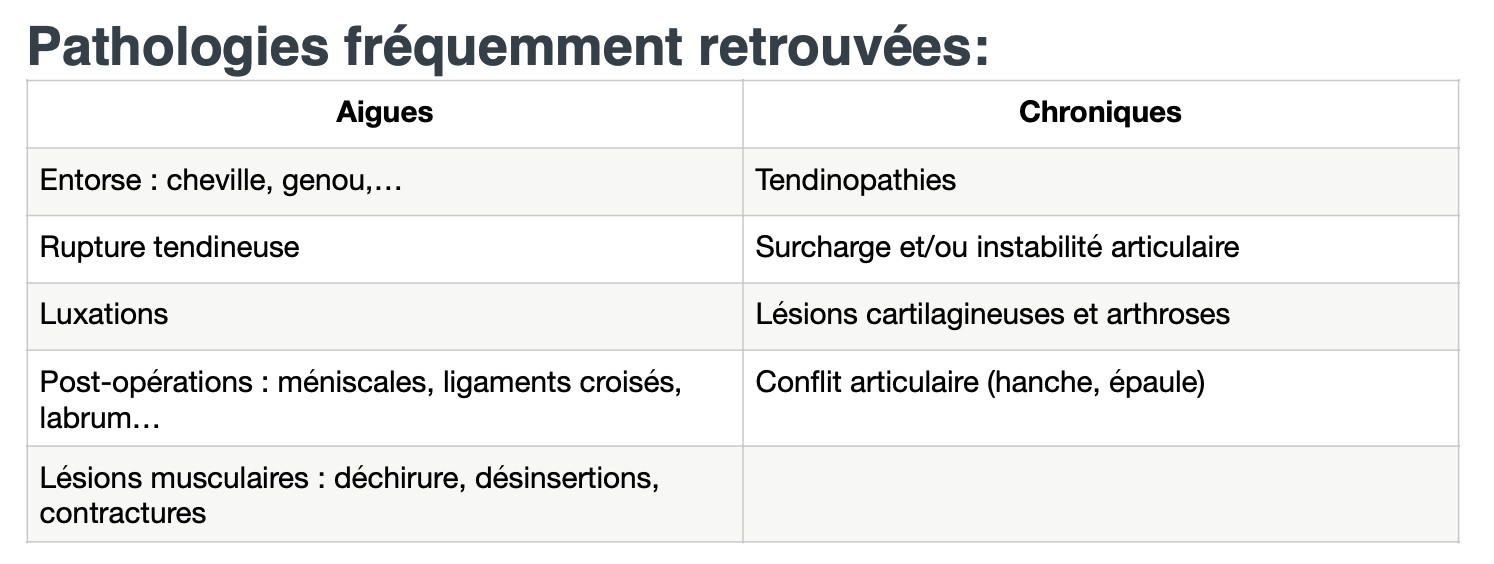
Pathologies
Here are some examples of common pathologies in sports practice
Injuries to the articular cartilage of the knee are common, posing an increasing public health problem, with multiple causes. Articular cartilage, different from meniscal cartilage, covers the bone ends of the femur and tibia, and allows the joint to slide-roll with low friction, absorbing the constraints applied to the joint.
The pain of osteoarthritis occurs when the articular cartilage of the knee loses its shape and function, deforms, thins, or disappears, with fibrillations and erosions, the appearance of osteophytes and bone remodeling. The 'chemical complex' of articular cartilage contains chondrocytes cells synthesizing the matrix. The matrix, with 65-80% water, and not vascularized, which does not facilitate healing, is composed of aggregates of proteoglycans (PG) linked to hyaluronic acid, and collagen fibers mainly of type II. The compliance and elasticity of the cartilage account for the role of proteoglycans. When the matrix of the cartilage is injured and breached, there is a decrease in PG, with an increase in cellular divisions of chondrocytes, therefore an increase in the synthesis of PG, and repair of the cartilage lesion:
Osteoarthritis worsens with age but with individual variations: the chondrocyte sees its capacity to restore the matrix decrease: by decreasing the synthesis of PG which are smaller and irregular. Moreover, the more chondrocytes divide, as a consequence of the repetition of cartilage injuries, the faster they will be in senescence, with premature cellular aging. Chondropenia: it follows from what precedes that repeated traumas and lesions, excessive joint use, accelerate cellular senescence (by increasing the divisions of chondrocytes), with loss of articular cartilage volume: this is chondropenia. While in the high-level athlete subjected to non-extreme training, the cartilage is thick, thickens, with high compliance and elasticity, the repetition of acute injuries, articular contact stress, cartilage defects, meniscal and / or anterior cruciate ligament lesions, will lead to chondropenia, a loss of articular cartilage, progressively over time, in the aging athlete, an evolution towards knee osteoarthritis. These effects are potentiated with age, obesity, malalignment (varus-valgus) of the knee and / or patella, menopause.
The boundary between chondral defect and knee osteoarthritis is therefore moving, dependent on age, level of activity, presence of malalignment, obesity, instability (ACL), meniscal capital, muscle strength: good strength with a good ratio between quadriceps and hamstrings absorbs the constraints applied on the joint, and is favorable to the prevention of non-contact trauma type pivot of the knee (ACL, meniscus and cartilage).
The sprained ankle is the most common reason for consultation in common traumatology. It represents, approximately 20% of sports injuries.
A sprain is a traumatic ligamentous injury caused by an indirect mechanism and not resulting in permanent or temporary loss of normal relationships between joint surfaces. This distinguishes a sprain from a dislocation, where the joint loses its normal relationships permanently; it is an exceeding of physiological and joint barriers.
Ligaments are stays stretched from one bone to another around or in the middle of the joint. Their role is to allow the joint surfaces to remain in good contact during movements. They are an articulated restraint and, together with the joint capsule, constitute the passive stability system, allowing the joint to adapt to different gravitational constraints to ensure joint stability together with the active, musculo-tendinous system. The injury can range from a simple stretch (mild sprain) to a complete rupture (severe sprain), passing through the tearing of some bundles (moderate sprain).
A sprain follows a false movement of the foot, which causes a sudden torsion of the foot inward or outward. The most classic mechanism is the inversion mechanism. This inversion occurs during a jump landing, on a misstep, or while running and causes the foot to turn on the outer edge beyond the physiological barrier, putting excessive tension on the lateral ligaments, which, under mechanical constraint, can go as far as to give way.
The ankle joint becomes overloaded, the ligaments stretch, and tiny tears occur. The small vessels can easily burst, causing the ankle to swell.
Classically, an ankle sprain corresponds to an injury of the external ligaments between the tibia, the talus, and the calcaneus.
Sometimes an ankle sprain can be accompanied by a fr
Each knee has two menisci: an internal meniscus and an external meniscus. The meniscus is a small fibrocartilage shaped like a "crescent moon" located between the femur and the tibia. It acts as a wedge, stabilizing the knee, and as a shock absorber, supporting 40% of the forces exerted on the knee. An isolated meniscal lesion does not significantly affect the stability of the knee as long as the ligaments are intact, but it increases the risk of arthritis later.
Traumatic meniscal lesions occur following:
- a sudden twist of the knee (sprain) that can occur in any circumstance: sports, fall, running, fast walking, sudden lifting from a squatting position...
- when the knee is overused without any obvious traumatic cause.
Under these conditions, the meniscus, whether internal or external, can crack or even tear. This tear can cause knee pain (usually on the inner side of the knee if it is an internal meniscus and on the outer side in case of an external meniscus lesion). Swelling of the knee may occur following an effusion, and the knee may even lock and no longer extend normally.
There are also meniscal lesions that occur outside any traumatic episode, often due to aging of the meniscus. This is a very common lesion. It should be considered in mature patients who present with progressive onset of internal knee pain. The evolution of pain is often cyclic with more or less long painful episodes that settle for a while before the reappearance of identical symptoms. This is a difficult diagnosis that usually requires additional tests such as radiography (arthrography) or MRI.
These meniscal lesions can sometimes be associated with cartilage wear at the level of the femur and tibia, which is osteoarthritis. It is important to specify this cartilage damage as it can be responsible for residual pain, and it can potentially worsen following meniscus removal.
Knee pain from meniscal lesions is treated by arthroscopy. One of the advantages of arthroscopy is that the surgeon can precisely target his gesture and perform the removal of the torn part of the meniscus (partial meniscectomy) and preserve all its healthy portion. In some indications, arthroscopy also allows repairing a meniscus by performing a suture.
The knee is a frequently injured joint. The rupture of the ACL is constantly increasing, usually occurring during athletic activities. The knee is a vulnerable joint, the stability of the ligaments and menisci decreases during flexion. Techniques for preventing ACL ruptures in athletes are described, using, for example, selective muscle strengthening of the hamstrings, plyometrics, and depending on the sport. The anterior cruciate ligament or ACL is made up of elastic fibers located in the middle of the knee and stretched between the femur and the tibia. The orientation of these fibers explains that its essential role is to prevent the tibia from moving forward relative to the femur as well as its rotation. It has a stabilizing role in the knee.
Knee ligament tears most commonly occur after a sports accident (football, skiing, jumping sports, combat sports…) but can also occur in any circumstance where the knee is subjected to a sudden sprain. The most commonly torn ligament is the anterior cruciate ligament (ACL), but other ligaments (lateral ligaments, posterior cruciate ligament) can also be injured. A torn ACL can cause effusion with knee swelling and, above all, knee instability that gives way during walking or sports activities. The patient can no longer use their knee with the same confidence as usual. Meniscal injuries can occur in association with a torn knee cruciate ligament. Over time, anterior instability due to ACL rupture can lead to meniscal and cartilage injuries with an increased risk of knee osteoarthritis. In case of anterior cruciate ligament rupture, daily life is mostly normal but the more physical or sports activity is important, the higher the risks of instability are (especially team and combat sports).
The posterior cruciate ligament (PCL) can also tear during a knee sprain or a violent impact on the front of the tibia. In this case, the knee can become unstable but less frequently than with an anterior cruciate ligament tear. However, the risk of medium-term osteoarthritis is higher.
Ligament repair
Simple suturing of the anterior cruciate ligament does not yield good results because the ligament, once torn, becomes necrotic and loses its mechanical properties, even if the fragments are brought together and sutured. It is necessary to replace the ligament with an equivalent structure. A natural tendon called an autograft or transplant taken from the patient's knee and used to replace the torn cruciate ligament must be used: this is ligamentoplasty. Arthroscopy allows the reconstruction of a torn anterior cruciate ligament by performing an autograft.
1. Complete ACL rupture
2. ACL location diagram
3. ACL ligamentoplasty
The two most commonly used techniques today are:
- The KJ autograft technique according to Kenneth Jones
involves harvesting a 10 mm diameter strip of patellar tendon with two bone fragments through an incision on the front of the knee about 5 cm long. This graft is then replaced inside the knee by arthroscopy and positioned in place of the torn anterior cruciate ligament.
- The 4-bundle DIDT technique
involves using a transplant constructed using two tendons from the inner side of the thigh harvested through an incision of 2 to 3 cm on the inner side of the leg. This graft is also replaced in the knee by arthroscopy.
These transplants are very strong and especially have elasticity and characteristics very close to those of the normal anterior cruciate ligament. In the long term, the performance of the two methods is analogous. The assembly is solid and allows immediate rehabilitation.
Minor Muscle Injuries
By definition, they can be diagnosed by a simple clinical examination, and ultrasound or MRI is unnecessary here, and in any case would not show any abnormality. When classified in order of increasing severity, we distinguish: cramps, then muscle soreness, then contractures and contusions
They are due to an intense and involuntary contraction of the muscle. It occurs suddenly and is accompanied by significant pain, which lasts only a few minutes, but nevertheless leaves a contracture in the days following its appearance. The cramp most often occurs during exertion but can also occur at rest. Treatment consists of stretching, followed by massages and the application of ice. Prevention involves hydration, the intake of minerals and stretching before and after sports practice.
Muscle soreness or delayed onset muscle soreness is also called DOMS (Delayed Onset Muscle Soreness). These are muscle pains occurring 12 to 48 hours after exertion. They usually disappear within 5 to 7 days. The pain is less severe and moreover affects groups of muscles. Although muscle soreness is included in the usual classification of an injury without anatomical lesions, it presents micro-lesions of the muscle fibers due to excessive eccentric contraction solicitations and/or a lack of adaptation to a training level (muscle not adapted to the intensity of training). The most severe muscle soreness is observed during downhill running, efforts against gravity or during the practice of maximal strength reinforcement. There is impairment of muscle function and is accompanied by an increase in the inability to produce maximal force and an increase in muscle stiffness, often observed during the first 4 days with muscle pain.
While some treatments seem to alleviate DOMS, none of them have yet demonstrated their real effectiveness, particularly in accelerating muscle regeneration. Treatment consists of alternating hot/cold baths and a moderate resumption of activity. The severity of symptoms related to muscle soreness could be limited by: maintaining good muscle flexibility, especially that of the muscle groups involved in the targeted physical activity, pre-conditioning the main muscle groups with a few high-intensity eccentric contractions one or two weeks before scheduling difficult sessions, using specific warm-up exercises for the main muscle groups.
As the name suggests, contracture comes from the exaggerated contraction of part of the muscle. The pain is first felt at the end of the exercise, during the rest phases. If the effort is continued, the muscle "stiffens" more and more; the pain becomes noticeable during the exercise and then very uncomfortable at the end of it. The athlete distinctly perceives a bothersome area. On examination, we generally find only one muscle, or even a single muscle bundle, indurated and painful. The ultrasound will reveal no abnormality. The contracture lasts for 5 to 10 days. The contracture may come from a reflex contraction aimed at protecting the muscle and the joint(s) involved following a significant stretch. The origin may also be significant muscle fatigue leading to disorders of certain molecules at the cellular level (calcium, potassium, magnesium). This pathology can finally be favored by a recent muscle injury (strain, tear, contusion...) which means that the muscle fiber is not fully functional.
Treatment consists of the use of ice packs, muscle relaxants and massages, physiotherapy and functional rehabilitation.
Unlike the previous pathologies, a contusion is a trauma caused by a direct impact on the muscle. (Fall on a barrier, blow to the muscle, crutch...). Following the trauma, the muscle may be more or less injured, the muscle fibers more or less damaged (crushing, tearing). A slight internal bleeding (intramuscular hematoma) or subcutaneous swelling may occur. The consequences can be relatively minor if the impact was light. Most often they do not prevent physical practice. On the other hand, in case of a severe blow, the muscle fibers may have suffered significant tearing equivalent to a tear, or even a muscle rupture. The pain is sudden and excruciating, causing a stop in activity. The important thing is to treat the hematoma in order to prevent it from preventing muscle healing and/or calcifying, which in both cases weakens the muscle fiber.
Severe muscle injuries
Here, the clinical examination remains important, but muscle ultrasound becomes indispensable to specify the type of injury, and thus, its treatment. However, it should not be performed too early. The ideal time is between the 48th and 72nd hour: indeed, the hematoma, resulting from damage to the muscle bundles, often only appears after a certain period of time, and an ultrasound performed too early risks missing more serious injuries than expected.
In order of increasing severity, we distinguish:
These are micro-tears in the muscle bundle, sometimes associated with simple fraying of myofibrils. They are caused by excessive demands on the muscle working at the limit of stretching. They are recognized by a sudden but moderate pain, poorly localized, causing relatively minor discomfort. The athlete has little pain when asked to perform movements alone, but stretching is painful, as is isometric contraction (during a resisted movement). Finally, note the absence of visible bruising. Palpation reveals a hardened cord. Ultrasound shows an elongated hypoechoic area.
Treatment must be immediate and allows recovery within 10 to 15 days thanks to containment such as elastoplast (tape), ice packs, rest, local anti-inflammatories, and other specific physiotherapy methods.
This time, it is tears of fibers, or even entire muscle bundles.
They are caused by two factors:
- Either by a too violent and too rapid contraction (type start)
- Or by an impact on a contracted muscle
They are recognized by a sudden and well-localized pain associated with a total inability to move. The muscle strain occurs during exertion and causes its immediate stop.
Of course, in this case, one would not even attempt any stretching or other maneuver because here the injury is too serious. The muscle strain is mainly seen in the hamstrings and the inner gemellus.
Moreover, a hematoma does not take long to appear. If the injury is superficial or interstitial, a bruise appears within a few days. It constitutes an element of good prognosis. If the injury is deep, intramuscular, the hematoma does not spread, the bruise is lacking, and the ultrasound shows it very well and can guide us towards a possible puncture. The treatment lasts from 21 to 30 days. It is also urgent to immediately apply a compressive containment completed by a splint, and to apply icing which can be prolonged for 21 days relayed by more specific methods of physiotherapy.
These are, unfortunately, the same problems, in the first case, the muscle is completely torn in its fleshy part, in the other case the tear occurs in its osteo-ligamentous insertion. Often there is an added snapping sound. They are caused by the same mechanisms as before: too violent and too brief effort or direct impact. The pain can go up to loss of consciousness, the injured person is totally impotent and a hematoma or swelling appears within a few hours which can mask the palpable notch of the fibers. The ultrasound confirms the true “fracture” of the muscle. The treatment lasts from 45 to 60 days during which strict immobilization must be respected (21 days) then a surgical opinion is systematically sought.
Traitement
"Rehab is training in the presence of an injury"
- Evaluer le risque de blessures et informer / entrainer le patient pour diminuer les risques d’apparition.
2. Exécuter les tests nécessaires en cas de blessures aiguës et agir en concéquence.
3. Entrainer le patient dans le respect des limites de cicatrisations / douleurs de la blessure en question
4. Améliorer les mouvements nécessaires au sport et imiter les conditions de compétitions + réévaluation
- Sportif amateur
- Sportif confirmé en cabinet ou sur le terrain
- Club / académie
- Thérapie manuelle
- Exercise therapy (renforcement, contrôle neuromusculaire, etc.)
- Analyse du mouvement et tests de force
- Accompagnement (taping, physiotherapie, éducation, etc.)
Concept intégré 2.0
Le C.O.S.L. (Comité Olympique Sportif Luxembourgeois) est plus que jamais déterminé à promouvoir dans les années à venir les activités physiques et sportives sous toutes ses formes et à rassembler, intégrer, écouter,... toute la société dans le processus afin que ce document stratégique soit non pas un guide “du milieu sportif élargi” mais un véritable concept intégré pour le sport au Grand-Duché du Luxembourg.
1) L'activité physique et sportive renforce notre société
2) Chaque membre de notre société exerce une activité physique régulière
3) Un plus grand nombre de Luxembourgeois sont compétitifs à un niveau international
Find a Physiotherapist
Locate a qualified physiotherapist near you from our network of over 1300 professionals.